 Who are we?
Who are we?
The Cardiology Lipid Management Service at ALMAR
The Advanced Lipid Management And Research (ALMAR) Centre has been established at Tallaght University Hospital (TUH) for the study and treatment of patients with complex cholesterol disorders. The Centre is led by Professor Vincent Maher, Consultant Cardiologist/Lipidologist and Irish representative on the Global Familial Hypercholesterolemia Network group.
High cholesterol is the major contributing factor for atherosclerotic heart disease worldwide. Our mission is to raise awareness regarding these dangers and identify those in Ireland at risk. Cholesterol measurements performed nationally in association with our trans-Ireland cycle completed in 2017, highlighted that 60% of individuals measured had some form of cholesterol disorder. Whilst the majority of lipid disorders can be managed and are being managed in primary care, the ALMAR centre aims to support primary care facilities in the assessment and management of patients with complex lipid disorders.
What do we do?
The ALMAR centre aims to support primary care facilities in the assessment and management of patients with complex lipid disorders. The Lipid Management clinic is held weekly on Friday mornings.
The ALMAR centre in TUH routinely see
- Patients with extreme cholesterol values LDL > 6.5mmol/l, TG >10mmol/l, HDL <0.5mmol/l.
- Patients who fail to show an effective response to treatment either due to the type and severity of their lipid disorder or their intolerance to lipid lowering therapy.
- Genetic Lipid disorders such as familial hypercholesterolaemia, familial combined hypercholesterolaemia. (Cascade screening of family members may also be facilitated).
- Patients requiring special investigations such as apolipoproteins, Lipoprint, DNA genotyping, or more detailed vascular assessment.
Referrals can be made to Professor Vincent Maher or the Lipid Nurse Manager Ruth Agar.
Lipid Nurse Manager: Ruth.agar@tuh.ie
ALMAR centre almar@tuh.ie
Telephone Contact: 01 414 2052
Why TUH?
There has been a tradition of Preventative Cardiology services based at TUH since its foundation. As a consequence, a number of the components required to initiate a dedicated advanced cholesterol management service are already in place. Close collaboration between the cardiology department, clinical biochemistry department, endocrinology department and vascular services has facilitated an ethos of preventative orientated strategies.
Many clinical trials and challenging problems in cholesterol related disorders have been managed effectively at TUH. It is therefore our hope to utilise all of these resources together with additional staff and diagnostics to further develop the ALMAR centre.
Section: What are lipids, lipoproteins and cholesterol?
Lipid is a collective term that refers to blood and cellular cholesterol, fats (Triglycerides) and phospholipids. Cholesterol is a fat-like substance that is found in all body cells. It is essential for cell membranes, some hormones, vitamin D and bile acids synthesis. The body is capable of synthesizing sufficient cholesterol for its needs but also acquires cholesterol from dietary sources.
To ensure its solubility, cholesterol travels through the bloodstream bound to proteins called apoproteins (e.g apo B) and the complexes are known as lipoproteins. These particles are arranged so that the hydrophobic fatty acids e.g. those in triglycerides, remain on the inside and the hydrophilic free cholesterol, phospholipid head groups and apoproteins lie on their surface. The main lipoproteins are Chylomicrons, Very low density lipoproteins (VLDL), Intermediate density lipoproteins (IDL), Low-density lipoproteins (LDL) which are apo B containing and High-density lipoproteins (HDL) which contain apo A-1. The pathways associated with the various lipoproteins are outlined in Figure 1. Essentially, dietary acquired cholesterol and triglyceride are used to form chylomicrons which deliver them to the liver. These in addition to those synthesized in the liver combine with apoproteins to form VLDL particles. They are broken down in the blood stream into VLDL remnants and IDL to form LDL particles. Cholesterol is returned to the liver by HDL particles from peripheral cells and is finally excreted in the bile.
The main lipoproteins associated with atherosclerosis are apo B containing VLDL remnants, IDL, and LDL whereas apo A-1 containing HDL Is considered protective in most instances. Having healthy levels of these lipoproteins is important. A high level of LDL ‘Lousy, Lethal’ cholesterol leads to plaque formation in the arteries. Conversely HDL “Healthy Hoover” cholesterol, transports cholesterol from around the body to the liver for removal.
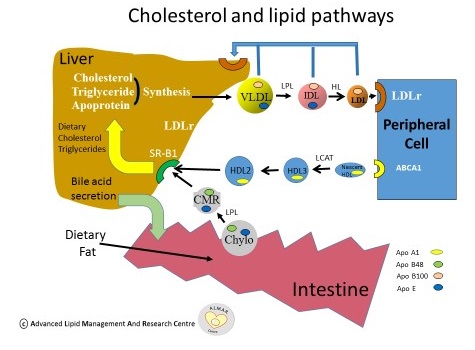
Figure 1: Cholesterol and Lipid Pathways
What is High Blood Cholesterol?
High blood cholesterol is a condition where excess cholesterol containing particles circulate in the blood stream. There are usually no signs or symptoms and therefore people are unaware that they have high cholesterol unless they have some obstructive cardiovascular disease. In those with high cholesterol or insufficient HDL cholesterol, they have an increased cardiovascular risk especially when associated with diabetes, obesity, high blood pressure and smoking.
Coronary heart disease is caused by plaque build-up resulting in atherosclerosis. Plaque consists of cholesterol, fat, calcium, and fibrous tissue. Over time, plaques grow and narrow the coronary arteries, which, may limit the supply of oxygen-rich blood to the heart. If a plaque ruptures, blood clot formation occurs and if large enough may reduce blood flow (angina) or completely block a coronary artery resulting in a myocardial infarction (MI). Plaque can also build up in other arteries in the body, such as those supplying the brain or limbs, resulting in problems such as transient ischaemic attacks, stroke or intermittent claudication
What causes high cholesterol?
There is a normally a well-balanced circulation of lipoprotein particles that help supply the building blocks and energy necessary for normal body function. Due to gene defects related to the enzymes, carrier proteins and receptors involved in lipoprotein transport, alterations in lipoprotein metabolism may occur. This can be particularly problematic when excess lipid is available due to over nutrition, excess body weight or hormonal imbalances.
Genetic Factors
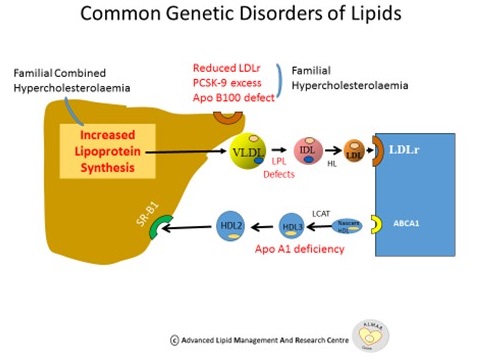
Numerous genes relating to enzymes, structural proteins and receptors influence lipoprotein levels in the body. See figure 2 . Disorders range from common, less common and relatively rare. The more prevalent disorders include Polygenic Hypercholesterolaemia and Familial Combined Hyperlipidaemia. Polygenic High cholesterol occurs where small effects from many different genes result in increasing cholesterol levels over time. Familial Combined Hyperlipidaemia (FCH) is due to variations in genes controlling lipoprotein synthesis or catabolism via the action of lipoprotein lipase. The latter may present with either elevated cholesterol, triglyceride or both in at least 2 family members, with a pattern that varies with time and is associated with premature cardiovascular disease. This disorder has a prevalence of 1:100 in the UK (1).
In Familial Hypercholesterolaemia (FH), patients can present with an LDL receptor mutation, increased production of Proprotein Sonvertase Subtilisin Kexin 9 (PCSK9) which reduces LDL receptor numbers, or an apoprotein B100 defect. Ultimately all 3 cause inadequate clearance of LDL, resulting in higher LDL plasma levels. FH is estimated to occur in 1:200 to 1:500 of the population and is associated with a high cardiovascular risk.(1) This is partly due to the life-long exposure of high cholesterol levels associated with these genetic disorders. If high cholesterol levels remain untreated, long term exposure accentuates the risk of premature MI and stroke. If the frequency of this condition in Ireland was 1:200, roughly 24,000 Irish people would suffer from FH of which approximately 90% are undiagnosed.
One of the main mechanisms by which HDL is anti-atherogenic is through reverse cholesterol transport. An apoprotein A1 deficiency, the main apoprotein in HDL, may result in decreased HDL levels possibly increasing cardiovascular risk.
Less common conditions include Type 3 Hyperlipidaemia due to the E2 E2 polymorphism in the Apo E gene that produces equimolar elevations in triglyceride and cholesterol in the presence of diabetes or insulin resistance. This occurs in 1:5,000 and is associated with premature vascular disease. (1)
There are rare disorders of chylomicron metabolism and HDL metabolism. According to Heart UK (1) those affected by Lysosomal Acid Lipase Deficiency (LALD)-a cholesterol storage disorder are estimated at 25 per million.
Hypertriglyceridaemia:
Hypertriglyceridaemia (HTG) is a feature of numerous metabolic disorders including dyslipidaemias, metabolic syndrome, and type 2 diabetes mellitus and can increase the risk of premature coronary artery disease. According to the literature, severe hypertriglyceridaemia is the most common cause of acute pancreatitis after gallstones and alcohol [3,4]. Patients with Triglyceride levels >10mmol/l are at risk of developing pancreatitis and warrant urgent review and assessment.
Modifiable Environmental Factors
Improving diet through modification of cholesterol, fat and alcohol intake, together with exercise and smoking cessation are important aspects to favourably modify lipid levels as indicated below.
Figure 2: Common Genetic Disorders of Lipids
References
- www.heartuk.org.uk
- Nordestgaard B., M. Chapman J., Humphries S., et al. for the European Atherosclerosis Society Consensus Panel. Familial hypercholesterolaemia is underdiagnosed and undertreated in the general population: guidance for clinicians to prevent coronary heart disease Consensus Statement of the European Atherosclerosis Society. EHJ (2013) 34, 3478–3490 doi:10.1093/eurheartj/eht 273
- Fortson MR, Freedman SN, Webster PD. Clinical assessment of hyperlipidemic pancreatitis. Am J Gastroenterol. 1995;90:2134–2139. [PubMed]
- Toskes PP. Hyperlipidemic pancreatitis. Gastroenterol Clin North Am. 1990;19:783–791. [PubMed]
Assessment and Management of Lipid Disorders
Assessment (Figure 3)
A careful and detailed clinical assessment is essential in order to assess individual risk of cardiovascular disease or in cases of severe hypertriglyceridaemia, a pancreatitis risk.
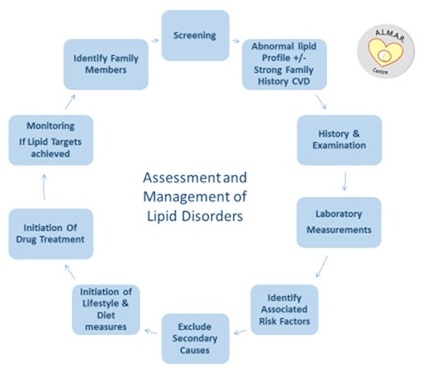
Figure 3: Assessment and Management of Lipid Disorders
History
While excess blood lipid levels do not cause any symptoms on their own accord, association with cardiovascular disease and pancreatitis may produce symptoms.
It is therefore important to elicit if the patient is complaining of symptoms that may suggest obstructive vascular disease such as
- Angina, shortness of breath or change in exercise tolerance may indicate possible CVD.
- Visual changes may indicate evidence/risk of TIA.
- Erectile Dysfunction in males – may serve as a marker for peripheral vascular disease. The risk becomes more pronounced with increasing age, indicating the need for monitoring.
- Abdominal pain, radiating to the back, nausea or vomiting may indicate a risk of pancreatitis.
Additional important information: Smoking status, alcohol intake and presence of diabetes should also be ascertained because of the associated greater risk from lipid disorders in these conditions. A history of premature heart disease in first degree relatives i.e. males <55 years or females < 60 years is also important as it highlights potential greater risk even when lipid levels are modestly raised.
Examination
- General Appearance, gender, race, body habitus, anthropometric measurements.
- Some types of hypercholesterolemia lead to specific physical findings. For example, familial hypercholesterolemia may be associated with xanthelasma (yellowish patches underneath the skin around the eyelids) corneal arcus (white/grey discoloration of the peripheral cornea) and xanthomata (yellowish cholesterol-rich deposits) of the tendons surrounding the fingers, knees and elbows.
- Blood pressure and signs of smoking (yellow staining of fingers) should be assessed.
- Physical signs of vascular disease such as carotid bruits and the presence or absence of pulses (dorsalis pedis/ posterior tibial) should be determined. Ankle Brachial Index (ABI) may be utilised to diagnose peripheral vascular disease. The index is the ratio of the systolic blood pressures in the legs compared to the arms. A low ratio indicates obstructive peripheral artery disease.
Laboratory Measurements:
A Full Lipid Profile (FLP), should be ascertained at the first visit preferably prior to treatment initiation. This can be completed within clinic or medical practices using the Cholestech LDX, a finger prick testing kit which can process results within minutes. The Cholestech LDX by Abbot has been validated at TUH as an accurate tool in point of care testing.
Lipid Profiles: To fast or not to fast….
The only reportable difference in the fasting and non-fasting population relates to triglyceride (TG) levels. A Danish population study (consisting of 92,000 participants) highlighted that the normal range of TG in the non- fasting population is 0.3 mmol/l higher than in the fasting patient. There were no significant differences between Fasting and Non fasting TC, HDL, LDL. (1). Since we are generally in a post prandial state most of the day, non-fasting lipid levels may better reflect our average lipid levels.
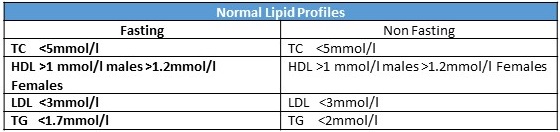
Table 1: Normal Lipid Profiles
Further laboratory measurements should include Liver and Renal profiles, Homocysteine, high sensitivity CRP, Hba1c to assess for diabetes, TFT to assess for hypothyroidism and Creatinine Kinase to assess for muscle damage in those with a history of muscular aches. Pancreatic amylase measurements should be considered for those with pancreatitis risk secondary to severe hypertriglyceridemia.
Designated Lipid centres such as the ALMAR centre at TUH have access to further risk marker measurements such as Apo A1, Apo B100, Lipid electrophoresis, Lipoprotein (a), Lp(a) and Lipoprint.
Lp(a) has been considered a cardiovascular risk factor for many years (2). It is a risk marker for CVD particularly when associated with elevated LDL levels (3). Ideally, Lp(a) measurements should be obtained to assess the overall cardiovascular risk.
Genetic testing may be considered in those with conditions such as Familial Hypercholesterolaemia to assess if there is a life-long burden from high cholesterol levels. In the future more genetic testing may guide on likelihood of treatment responses and sub categories of patients at greater risk.
Identify Associated Risk factors
Although dyslipidaemia is considered the most important risk factor for cardiovascular disease, its risk is significantly modified by associated risk factors including Diabetes, Smoking, Hypertension, Family history of high cholesterol and a Strong Family history of premature CHD in Males < 55 and Females < 60 years.
Exclude secondary causes of dyslipidaemia
When assessing risk and assigning lipid targets for individuals with dyslipidaemia, secondary causes of dyslipidaemia should also be investigated. Acquired hyperlipidaemias often mimic primary forms of hyperlipidaemia and can have similar consequences. Diabetes mellitus, Hypothyroidism, Nephrotic syndrome, Chronic renal failure, high alcohol consumption, medications such as thiazide diuretics, beta blockers, Estrogens, some rare endocrine disorders and metabolic disorders may significantly affect lipid levels. It is important to exclude secondary causes and treat these conditions to allow the underlying lipid disorder be detected.
Assessing Risk
Risk charts such as Systematic COronary Risk Evaluation (SCORE) are intended to facilitate risk estimation in apparently healthy persons with no signs of clinical or pre-clinical disease. (4) SCORE assesses CVD risk using five variables; gender, smoking status, age, systolic blood pressure and total cholesterol. There are different charts for low risk and high risk countries. Ireland is designated as a low risk country.
Based on these scores, individuals are categorised as having Low, Medium, High and very high risk. Those who have diabetes, renal disease or proven vascular disease are already considered as having a very high risk. Based on an individual’s cardiovascular risk, targets for LDL cholesterol are recommended as indicated below.
Lipid Targets
High risk: <2.6mmol/l Very high risk: <1.8 mmol/l
Management
Modifying factors such as diet and exercise will always play a key role within lipid management but those with complex disorders who are not reaching target will require medication management. Even for individuals with known high cholesterol, challenges may exist due to poor treatment response rates, drug intolerances and co-existing disorders which may hamper treatment.
Initiation of Lifestyle and Dietary Measures
Lifestyle:
Increasing activity: Being sedentary is linked to low HDL ‘Good’ Cholesterol levels. The WHO guidelines (5,6) recommend that Adults aged 18–64 should do at least 150 minutes of moderate-intensity aerobic physical activity throughout the week or do at least 75 minutes of vigorous-intensity aerobic physical activity per week or an equivalent combination of moderate- and vigorous-intensity activity.
Smoking Cessation: Smoking lowers HDL cholesterol and damages your arteries and blood vessels, which increases risk of plaque formation. As health professionals, we know that smoking is bad for your health but a combination of smoking and high cholesterol is especially dangerous to your heart. If you smoke and have high cholesterol, you have a much greater risk for heart attack and stroke than if you have only one of following risk factors: Hypertension, Diabetes and a strong family history of early CVD.
It is vital that we offer our patients full support in smoking cessation whether that be in the form of medication and/or referral to support services such as the HSE’s www.quit.ie programme.(7)
Diet:
Eating unhealthily: Consuming high amounts of saturated fats or trans-saturated fats can result in elevated LDL ‘bad’ cholesterol. Consuming polyunsaturated vegetable or marine fats reduces LDL cholesterol but also HDL cholesterol whereas monounsaturated fats lower LDL without adversely affecting HDL cholesterol levels. Diets containing higher concentrations of mono-unsaturated fats are best to help improve lipid levels.
Alcohol consumption: drinking too much can elevate triglyceride levels. According to the HSE, Low risk weekly guidelines for adults are: up to 11 standard drinks a week for women, and up to 17 standard drinks a week for men. (8) However for those with complex lipid disorders such as severe hypertriglyceridemia, the risk of developing pancreatitis is high. In severe cases, patients are advised to avoid alcohol consumption altogether or have a minimal intake.
Plant Stenols/Sterols
Plant stenols/sterols reduce LDL-cholesterol levels in the blood by reducing the amount of cholesterol absorbed from the intestine. These are quite effective with Benecol lowering cholesterol by an average of 14% and Flora Proactive lowering LDLc by approximately 10%. (9)
Red Rice yeast has LDL lowering properties similar to statins. Red Rice yeast contains the HMG-CoA reductase inhibitor lovastatin, which forms naturally when the rice yeast is fermented. It is important to realise the statin content of these products if patients are also taking statin drugs. They may be at a greater risk of myopathy when consuming both.
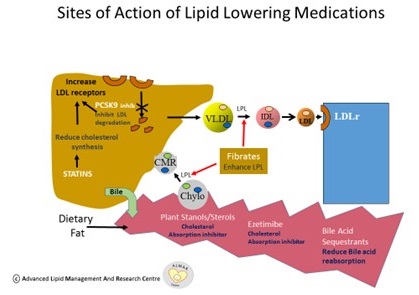
Initiation of Drug Treatment (Figure 4)
Statins:
Statins lower cholesterol by inhibiting HMG Co A reductase the rate limiting enzyme in cholesterol synthesis. Interestingly, this pathway is shared by Co Enzyme Q10 production and statins can also lower Co Enzyme Q 10 levels in muscles. Statins were originally derived from yeast e.g. Lovastatin, Simvastatin and Pravastatin and have a short half-life. However subsequently Atorvastatin and Rosuvastatin were directly synthesized and are more potent given their longer half-lives.
The Cholesterol Treatment Trialists Collaboration (CTTC), which reviewed over 90,000 participants, clearly demonstrated the benefits for individuals (with or without history of CVD) who were prescribed statins. Not only were they shown to significantly lower LDL cholesterol levels, but for every 1mmol/L drop in LDL cholesterol there was 22% reduction in CV risk. (10)
Statin intolerance:
As the name suggests, statin intolerance occurs when a patient is unable to continue to use a statin, either because of the development of a side effect or because of evidence of abnormal Liver function test or Creatinine Kinase levels.
In clinical trials, where patients were either given a statin or a placebo under blinded conditions the side effects reported were similar in both groups, suggesting that statins were generally well tolerated by the study populations.(11) Ninety present of those re-challenged with statins were able to tolerate these medications. It is our practice to discontinue statins for a period of 1 month, administer Co Enz Q10 100 mg once daily and reintroduce low dose statins to circumvent these problems.
Ezetimibe:
Ezetimibe reduces blood cholesterol by inhibiting the absorption of cholesterol by the small intestine. The 2005 IMPROV-IT trial highlighted that among individuals with recent Acute Coronary Syndrome (ACS), the addition of ezetimibe to moderate-intensity statin therapy is associated with a reduction in CV mortality, major CV event, or nonfatal stroke when compared to statin therapy alone. (12).
Fibrates:
Fibrates are utilised in the management of Hypertriglycerideamia. Fibrates lower blood triglyceride levels by reducing the liver's production of VLDL and by speeding up the removal of triglycerides from the blood. By activating lipoprotein lipase, fibrates also reduce the amount of small dense LDL.
Fenofibrate Intervention and Event Lowering in Diabetes (FIELD) trial was the largest cardiovascular prevention trial using fibrates in type 2 diabetes. The Field Trial highlighted that fenofibrate therapy reduced or delayed non-fatal myocardial Infarctions and revascularisation procedures, but had no effect on total mortality. Fenofibrate reduced diabetes-specific renal and eye disease however statins remain first line treatment for diabetic dyslipidaemia. (13)
The Action to Control Cardiovascular Risk in Diabetes (ACCORD) Trial of 2010 highlighted that the combination of fenofibrate and simvastatin did not reduce the rate of fatal cardiovascular events, nonfatal myocardial infarction, or nonfatal stroke, as compared with simvastatin alone. The ACCORD results do not support the routine use of combination therapy with fenofibrate and simvastatin to reduce cardiovascular risk in the majority of high-risk patients with type 2 diabetes. (14)
Bile Acid Sequestrants
Cholesterol is involved in the production of Bile. Bile acid sequestrants bind to bile acids in the terminal ileum preventing their reabsorption into the blood. This action results in reduced bile acids and the liver in response enhances bile acid synthesis by increasing the uptake of LDL cholesterol from the blood stream.
Considerations for treatment with PCSK9 Inhibitors:
In 2003, PCSK9 was first identified. It was noted to accelerate LDL receptor degradation. In 2005, a PCSK9 loss of function mutation was reported to cause a life-long decrease in LDL-C levels (15,16). Following this information, antibodies were developed to inhibit PCSK9. These inhibitors comprise fully humanised monoclonal antibodies and bind circulating free PCSK9. Inhibiting PCSK9 in this manner prevents degradation of LDL receptors leading to increased clearance of LDL, resulting in lower LDL plasma levels.
Recent trials utilising two of these PCSK-9 inhibitors have been completed. The Fourier trial utilised Evolocumab on top of statin treatment in patients with non–acute coronary artery disease and reduced LDL cholesterol levels to 0.78 mmol/l (17). This resulted in a 15% reduction in CV events. Subsequently, the Odyssey Outcomes trial (18) involved using Alirocumab on top of statin treatment in patients with acute coronary syndromes resulting in LDL cholesterol reduction to 0.5 mmol/l and a further 15 % reduction in cardiovascular events. As a result, in those with statin intolerance or non-achievement of lipid targets despite maximal lipid-lowering treatment, consideration needs to be given to the use of PCSK-9 inhibitors. Current utilisation is by an early access programme (EAP) only. Access to PCSK9 treatment was based on the National Institute for Clinical Excellence (NICE) guidelines in relation to primary and secondary prevention for patients with persistently elevated levels of LDL >4mmol/ with high risk CVD and >3.5mmol/l with very high risk CVD respectively, despite maximum tolerated oral treatment. PCSK9 inhibitors, Alirocumab and Evolocumab are deemed high tech drugs therefore prescribing guidelines and drug availability are currently under review by HSE reimbursement.
Management of Severe Hypertriglyceridaemia
Individuals with markedly elevated triglyceride levels e.g exceeding 10 mmol/ls have a high risk of developing acute pancreatitis. The culprit lipoproteins are usually chylomicrons as these large particles can become stuck in the pancreatic capillary network and induce localised inflammation. Without appropriate intervention, these individuals can have recurrent hospitalisations and potentially ICU admissions. A combination of increased chylomicron synthesis from excess fatty acid availability and reduced chylomicron clearance may be responsible. In those at risk, it is therefore important to minimise fatty acid availability. By reducing dietary fat intake and reducing weight, fatty acid release from adipose tissue is limited. Exercise also improves insulin sensitivity and reduces adipose tissue fatty acid release into the circulation. In addition, clearance of these particles can be enhanced by improving lipoprotein lipase activity with exercise and the use of the fibrate drugs. Newer therapies are awaited to reduce chylomicron production.
Figure 4: Sites of Action of LLT
Monitoring if Lipid Targets achieved
Although reduction in cholesterol levels may be seen within two weeks of initiated therapy, patients are invited to attend for blood sampling after three months to ascertain control on current lipid lowering therapy and whether LDL targets based on risk have been achieved.
Screening
Once complex lipid disorders are identified in patients, it is important that family members are identified and screened accordingly with an aim to reducing overall risk of developing CVD. Family cascade screening may help identify patients at an earlier age, increasing the proportion of individuals with complex lipid disorders receiving timely and appropriate treatment (20). National screening is important to identify individuals early. We have performed a preliminary snapshot of lipid levels in Ireland (21) to pave the way towards a more comprehensive lipid audit in Ireland. A careful and detailed clinical assessment is essential in order to assess individual risk of cardiovascular disease or in cases of severe hypertriglyceridaemia, a pancreatitis risk.
References:
- Nordestgaard et al. EAS EFLM joint ConsensusPanel. EurHeart J 2016; online April 26
- European Heart Journal Advance Access: Lipoprotein(a) as a cardiovascular risk factor published October 21, 2010. doi:10.1093/eurheartj/ehq386
- Vincent M. G. Maher, B G Brown, S M Marcovina, LA Hillger, X Q Zhao, J J Albers: Effects of lowering LDL cholesterol on the cardiovascular risk of lipoprotein (a). JAMA The Journal of the American Medical Association 12/1995; 274(22):1771-4., DOI:10.1001/jama.1995.03530220037029
- European Heart Journal (2016): ESC/EAS Guidelines for the management of dyslipidaemias. 32, 1769–1818. doi:10.1093/eurheartj/ehr158
- http://www.who.int/dietphysicalactivity/factsheet_adults/en/
- http://www.who.int/mediacentre/factsheets/fs385/en/
- www.quit.ie
- HSE Alcohol Partnership Policy 2015: HSE Health and Wellbeing Alcohol Misuse Group
- Reduction of Serum Cholesterol with Sitostanol-Ester Margarine in a Mildly Hypercholesterolemic Population Tatu A. Miettinen, M.D., Pekka Puska, M.D., Helena Gylling, M.D., Hannu Vanhanen, M.D., and Erkki Vartiainen, M.D.
- CTTC. The effects of lowering LDL cholesterol with statin therapy in people at low risk of vascular disease: a meta-analysis of individual data from 27 randomised trials. Lancet 2012;380(9841):581-590.
- Finegold JA, Manisty CH, Goldacre B, Barron AJ, Francis DP What proportion of symptomatic side effects in patients taking statins are genuinely caused by the drug? Systematic review of randomised placebo-controlled trials to aid individual patient choice. European Journal of Preventive Cardiology 2014 21: 464
- Cannon CP, et al. "Ezetimibe Added to Statin Therapy after Acute Coronary Syndromes". The New England Journal of Medicine. 2015. 375(25):2387-2397.
- Practical Diabetes Int 2006; 23(3): 135–137 Resins the FIELD trial
- Effects of Combination Lipid Therapy in Type 2 Diabetes Mellitus. The ACCORD Study Group The New England Journal of Medicine April 29, 2010.
- Karatasakis A, Danek BA, Karacsonyi J, et al. Effect of PCSK9 Inhibitors on Clinical Outcomes in Patients With Hypercholesterolemia: A Meta‐Analysis of 35 Randomized Controlled Trials. Journal of the American Heart Association 2017; 6:e006910.
- Horton JD, Cohen JC, Hobbs HH. PCSK9: a convertase that coordinates LDL catabolism. Journal of lipid research 2009; 50:S172-S7.
- Sabatine MS, Giugliano RP, Keech AC, et al, Evolocumab and Clinical Outcomes in Patients with Cardiovascular Disease. , N Engl J Med. 2017 May 4;376(18):1713-1722.
- www.acc.org/latest-in-cardiology/clinical-trials/2018/03/09/08/.../odyssey-outcomes
- Maurice J O'Kane, Ian B Menown, Ian Graham, Vincent Maher, Gerald Tomkin, Paul Nicholls, Colin Graham: The Detection of Heterozygous Familial Hypercholesterolemia in Ireland. Advances in Therapy 05/2012; 29(5):456-63., DOI:10.1007/s12325-012-0021-0
- Agr R., Markham C., Prendergast M., Canning R., Maher E., Finn C., Sammon N., Fall S., Fallon N., Hanrahan E., King L., Maher V. A snapshot of lipid levels in the republic of Ireland in 2017.
- Murphy C, Shelley E, O'Halloran AM, Fahey T, Kenny RA. Failure to control hypercholesterolaemia in the Irish adult population: cross-sectional analysis of the baseline wave of The Irish Longitudinal Study on Ageing (TILDA). Ir J Med Sci. 2017 Mar
Achievements to date
1/Establishment of Irish Lipid Network
The Irish Lipid Network has over 80 members and provides vital links to experts throughout the country with specific interest in Lipid Management and in moving the Lipid agenda forward. The Irish Lipid network is led by Professor Maher and meets quarterly.
For further information please contact ruth.agar@tuh.ie
2/Completion of the National Lipid Services Survey 2017
The aim of the survey was to identify the personnel, resources and services currently available within hospitals throughout the country. The second aspect of the survey was to ascertain lipid measurements performed by hospital laboratories in 2016. Just over 1.7 million equating to 39% of the population were tested that year.
The National Lipid Services Report is due to be published in the summer 2018
3/ALMAR centre Lipid Disorders Registry Development
A registry carries many benefits for the individual with complex Lipid disorders. The
primary goal of developing such a registry is to manage and treat patients effectively, collate further information on the complexity of disorders, increase awareness of the prevalence of Lipid disorders, identify shortcomings in the healthcare delivery system, predict future needs and areas of concern and finally empower Physicians and organisations such as the ALMAR centre at TUH to lobby effectively on behalf of people with complex Lipid disorders.
4/ALMAR Fundraising and Awareness event 2017

Professor Maher and colleagues cycled the length and breadth of Ireland in the summer of 2017 in order to raise awareness and vital funds to develop the ALMAR centre. Cholesterol testing in the non-fasting population occurred at five sites across the country highlighting lipid abnormalities in 60% of the population. (Based on abnormal concentration ranges in the non-fasting population from the Nordestgaard Danish study 2016). The snapshot of cholesterol trends in Ireland argues strongly for a larger appropriate population study.
Publications:
1/ ‘A snapshot of lipid levels in the Republic of Ireland in 2017’ has now been published by the Irish Journal of medical science and is available to view here: https://link.springer.com/article/10.1007/s11845-018-1820-3
2/ ‘Latest Evidence on Lipid Management’ 2017.E.Egom, H. Shiwani and V.Maher
https://issuu.com/greencrosspublishing/docs/update_cardiology_issue_4_2018
3/ ‘Lipid, Lipoprotein and Cholesterol management in Clinical Practice’ Issue 4 Volume 11 May/June 2018 Nursing in General Practice - the journal of the Irish Practice Nurses Association.
Coming Soon:
1/ National Lipid Survey Report 2017
3/ ‘Estimating the prevalence of lipid disorders in Ireland utilising hospital laboratory values’
Donations
Ongoing funding is required to further develop this pioneering centre, in particular website development which aims to provide education for medical and lay personnel and promote heart health for numerous people in our community with significant cholesterol disorders.
By donating your contribution will enable us to continue the development of this specialised cholesterol management centre.
We are grateful for your generosity and most importantly your commitment to our mission in tackling the damage caused by cholesterol.