March 9th 2018
The Hospital announced a formal name change to Tallaght University Hospital. The change of title reflected the of the Hospital's position as one of the country's leading academic teaching hospitals. The evolution of Tallaght Hospital to Tallaght University Hospital formalises our status as one of the country's major academic teaching hospitals that continues to be at the forefront of innovative research. June 21st 1998
On June 21st 1998, 115 patients were transferred to Tallaght from the Adelaide, Meath and National Children's Hospitals in Dublin's city centre. This move happened after months of planning and detailed logistics. During the course of the day 12 Eastern Health Board ambulances transported patients, accompanied by our medical and nursing staff, from the city centre to Tallaght along a planned route via South Circular Road, the Naas Road and the Belgard Road. Intensive Care (ICU) and Coronary Care (CCU) patients were transferred to Tallaght in a high-tech ambulance with its own mobile intensive care unit called MICAS. A team of medical and nursing staff was on stand-by at the Meath Hospital, National Children’s Hospital in Harcourt Street and in Tallaght throughout the transfer of patients. Prior to opening day, a removal company was hired to pack and move furniture, equipment and files: over 170,000 patient records and almost 50,000 patients' X-Rays. The move to Tallaght was a carefully-planned and extremely smooth-running operation thanks to the huge effort from staff and volunteers. From 23rd June, new patients were admitted to the Hospital and clinical activity built up steadily. Planning for the move
Planning for the Tallaght development began in 1981 when the Department of Health appointed the Tallaght Hospital Board to oversee the planning, building and equipping of the Hospital. In 1985, architectural competition results were published, with Robinson Keefe Devane Architects being appointed to design the new Hospital. Construction was approved in 1993 and building commenced in October of that year. Construction was completed in 1998. The Hospital was established under a Charter, agreed in Dail Eireann, on 1st August 1996. Today, Tallaght is a public, voluntary, teaching Hospital, funded by the Health Service Executive. | The Building
At a capital cost of £140M, the new development at Tallaght was one of the largest capital investments in healthcare ever undertaken by the State. Children, adults and older people are cared for at the hospital, which has 562 beds, 12 theatres, and 14 Critical Care beds. Built on a 35-acre site, the Hospital’s main corridor, Hospital Street, is 353.1 metres long - about a quarter of a mile. It is a unique challenge, bringing together over 600 years of medical and nursing care and education from the very different traditions of the Adelaide Hospital, the Meath Hospital and the National Children's Hospital (Harcourt Street). | The Adelaide Hospital
The Adelaide Hospital was founded in 1839 to serve the disadvantaged Protestant population of Dublin. Like the Meath and National Children's Hospitals, the Adelaide Hospital was run on a voluntary basis - its survival dependent on the generosity of others and the dedication of its staff. Famous for its nursing school, which was founded in 1859 by Miss Bramwell who had worked with Florence Nightingale in the Crimea, the Adelaide has been at the forefront of many medical advances. It was, for example, the first general hospital in Dublin to introduce a skin clinic (in 1868), a gynaecological unit (in 1868) and the bacteriological control of milk (in 1904). | The Meath Hospital
The Meath Hospital is the oldest of the three hospitals, founded in 1753. Situated in the ‘liberty’ of the Earl of Meath, the Hospital was opened to serve the sick and poor in the crowded area of the Liberties in Dublin. In the 19th Century the Meath Hospital achieved world-wide fame as a result of the revolutionary teaching methods and groundbreaking research carried out by Graves and Stokes, physicians of the Hospital. In more recent times, the Hospital developed specialised services in the fields of urology, psychiatry, orthopaedics, haematology, endocrinology and nephrology. | The National Children's Hospital
In 1821 a number of eminent Dublin doctors - concerned with the lack of treatment available for sick children in the city - founded the National Children's Hospital. It was the first hospital devoted exclusively to the care and treatment of sick children in Ireland and Britain. Indeed, one of the hospitals’ early students, Dr. Charles West, returned to London and founded Great Ormond Street Hospital in 1852. |
|
Directors of Tallaght University Hospital BoardIn accordance with bye laws made in November 2014 under the Tallaght University Hospital Charter, the Board of Tallaght University Hospital consists of an 11 Member Non-Executive Board. The Chief Executive and appropriate members of the Executive Management Team attend and participate fully in all Board meetings. Non-Executive Directors
Professor Anne Marie Brady (Chairman)
Dr. Vivienne Byers
Mr. John Hennessy
Mr. Mark Varian (Vice Chairman)
Dr. Darach Ó Ciardha
Mr. Mike Beary
Dr. Martin Lyes
Ms. Darina Barrett
Mr. Tom Lane
Reverend David Bowles
Senior Management in attendance at Board Meetings
Mr. John Kelly, Interim Chief Executive
Mr. Dermot Carter, Director of Finance
Prof. Peter Lavin, Clinical Director Medical Directorate
Prof. Catherine Wall, Director Quality Safety & Risk Management
Dr. Mary White, Chair of the Medical Board
Ms. Bridget Egan, Clinical Director of Peri-Operative Directorate
Ms. Aine Lynch, Director of Nursing & Integrated Care
Ms. Sharon Larkin, Director of Human Resources
Mr. Shane Russell, Chief Operations Officer Board Secretary - Ms. Anne McKenna Board Agendas & Minutes Please note that all Board Agenda’s and Minutes prior to 2023 have been archived Hospital Board Agenda - 28th April 2025
Hospital Board Minutes - 28th April 2025
Hospital Board Agenda - 31st March 2025
Hospital Board Minutes - 31st March 2025
Hospital Board Agenda - 27th January 2025
Hospital Board Minutes - 27th January 2025
Hospital Board Agenda - 25th November 2024
Hospital Board Minutes - 25th November 2024
Hospital Board Agenda - 21st October 2024
Hospital Board Minutes - 21st October 2024
Hospital Board Agenda - 30th September 2024
Hospital Board Minutes - 30th September 2024
Hospital Board Agenda - 29th July 2024
Hospital Board Minutes - 29th July 2024
Hospital Board Agenda - 27th May 2024
Hospital Board Minutes - 27th May 2024
Hospital AGM Board Agenda - 27th May 2024
Hospital AGM Board Minutes - 27th May 2024
TUH Board Corporate Governance Manual - July 2024
The corporate governance manual provides members of the TUH Hospital Board with the information they need about corporate governance to perform their duties to the highest standards of accountability, integrity and propriety. It sets out the systems and procedures by which the Hospital Board directs and controls its functions and manages its business. You can read the manual through this link. The additional list of relevant legislation and regulatory provisions is considered under the Charities Governance Code.
It is the responsibility of the Tallaght University Hospital (TUH) Board to determine the Hospital’s risk appetite that it is willing to undertake in achieving its strategic objectives. The Board of TUH undertook a Risk Appetite Review in 2023 and the Risk Appetite Statement sets out the risk tolerance for TUH.
|
Tallaght University Hospital (TUH) is committed to ensuring the privacy and confidentiality of your personal information. This page sets out how the hospital will handle your personal information. If you require additional information, you can read our Data Protection Statement by clicking here. Legal BasisIn processing your personal information, TUH must comply with legislation which includes, but is not limited to, the General Data Protection Regulation (GDPR), the Data Protection Act 2018 and the Freedom of Information Act 2014. We are committed to complying with all applicable privacy laws which govern how TUH collects, uses, discloses and stores your personal information. What is Information Governance?Information governance is the set of standards we must follow in handling personal healthcare records. Good information governance means that all personal health information is handled legally, securely, efficiently and effectively, in order to deliver the best possible care to people who use our services. It also includes, where appropriate, the sharing of relevant personal health information with our healthcare providers. What does it involve?
Information governance at TUH covers a number of areas and activities. These include the following: - We must manage our records efficiently and effectively.
- This means that information should be accurate, up-to-date and accessible when it is needed
- We must ensure that information is kept securely and is accessed only by those who should be accessing it.
- We must protect the confidentiality of the information.
Information provided in confidence should not be used or disclosed in a way that might identify an individual without their consent and/or a legal basis for processing - Patients have a right to access health information about themselves
For further information on how to do so, please click here
Why do we need information about you?In order to provide you with the highest quality of healthcare, TUH needs to keep records about you. These records may include the following information: - Personal information
For example your name, date of birth, next of kin, contact details etc. - Contacts we may have had with you
For example, information on clinic visits, hospital admissions etc. - Notes and reports on your health
For example, information on treatment and care you need and/or may have received either directly from us or from other care providers such as a primary care team or your own GP - Results of investigations
For example, X-rays, blood tests etc.
What will we use your information for?Our staff who provide healthcare to you will use this information in a number of ways. These include, for example, to: - Confirm who you are when we contact you or when you contact us
- Make decisions about your ongoing care and treatment
- Make sure your care is safe and effective
- Check the quality of your care
- Ensure a safe care journey through our hospital and onto other care providers if required
Do I have a choice? If you want to receive safe and appropriate care and treatment at TUH, we must maintain an accurate record of relevant information about you. If you have concerns, however, about providing information, or how we share this information with our healthcare providers, please discuss this with our staff so you fully understand the impact on your care or treatment. Do you share information about me with anyone?In providing care, we may share relevant information about you with other organisations. These include, for example, - Other hospitals that are involved in your care and treatment
- Your GP
- Community Healthcare services
- Local authorities
- Primary care
- Pharmacy
When we do share your information with other organisations involved in your care, we do so under formal agreement about how it will be used, kept confidential and safe. We will not disclose your information to any other third party without your permission unless there are extenuating circumstances (for example, if the health and safety of others is at risk, if there is a legislative requirement for us to pass on information, etc.). Information may also be used in non-clinical ways. These include, for example, to - help manage finances (for example, billing, costings, etc.)
- teach and train our staff
- manage and plan our services
- perform clinical audits
- help investigate concerns or complaints that you and/or your family may have about your healthcare
Wherever possible, TUH uses information that would not identify you personally. In this way, it aims to use anonymous information. Do you use my information for research?TUH is an academic teaching hospital associated with Trinity College Dublin (TCD). We support and promote research activity throughout our hospital. Most importantly, research plays a vital role in the development of healthcare and the health services we deliver. Our Research Ethics Committee must approve research before it takes place. If we wish to use your personal information for research, we will ask you for permission first. You will not be identified in any published research or results without your agreement. Can I see the information you hold about me?You have the right to access information TUH holds about you. The GDPR, the Data Protection Act 2018 and the Freedom of Information Act 2014 all allow for you to access the information we hold about you. You may access a copy of your personal healthcare records in either of two ways. These are as follows: For information on accessing your personal information under data protection legislation, please click here. For information on accessing your personal information under the Freedom of Information Act 2014, please click here. Data Protection Officer (DPO)TUH has a Data Protection Officer (DPO). Should you have any questions about how TUH uses your information, or you are concerned about any issue relating to your personal data, you may contact the DPO in any of the following ways: | By post: | Data Protection Officer
Tallaght University Hospital
Tallaght
Dublin 24
D24 NR07 | | By email | dpo@tuh.ie |
|
Tallaght University Hospital (TUH) is committed to promoting the safety and wellbeing of all children in our care. Child protection is the responsibility of all staff and to support this there are a number of mechanisms in place. The Hospitals practice is informed by Children First: National Guidance for the Protection and Welfare of Children, DOH 2017. The guidelines for practice currently in TUH are a collaborative set of guidelines that are underpinned by the National Guidance. It is mandatory for all staff to be familiar with these guidelines and complete HSE Children First training. TUH has an active Children First Implementation Committee chaired by the Deputy Chief Executive. TUH also complies with the Garda Vetting requirements in the recruitment of staff to the Hospital. TUH will continue to strive to ensure all Children are cared for in a safe, secure and caring environment. Copies of the TUH and CHI at Tallaght Safeguarding Statements are available via the following links: TUH Adult Service / CHI at Tallaght. If you have any queries regarding child protection in the Hospital please contact the Hospital Social Work Department on 01 414 2462. This line is open from 9am-5pm Monday to Friday.
|
Established in 2013 the Patient Community Advisory Council (PCAC) was set up with the support of the Executive Management Team of TUH. The PCAC is dedicated to the improvement of quality in patient care at TUH and help support the Hospital’s values.
The group meets eight times a year provides an opportunity for the Hospital to hear directly from patients, users of our services on their experience during their patient journey with the Hospital. Provide feedback on current systems and processes in the Hospital and give their thoughts on new systems being introduced and generate new ideas to improve the standard of care.
The PCAC is composed of groups representing the Community along with staff of the Hospital.  | Declan Daly - Patient Representative & Chair of the PCAC |
Declan has a MBs in Co-operative and Social Enterprise and has worked in the financial sector for over 20 years in both voluntary capacity and also as a CEO. Due to a long term chronic health condition, Declan became involved with the Living Well Programme as a participant, became a Volunteer Leader and has now completed his Master Training in Chronic Disease Self-Management and Cancer Thriving and Surviving. Declan has now shifted his focus to the Community Sector and is currently the Lay Co-Coordinator for the Living Well Programme with Fettercairn Community Health Project. Declan brings his understanding of the difficulties associated with reduced mobility to the PCAC and has the ability to articulate the voice of members within his community who have similar mobility issues. Declan is committed to improving the role of the community in the development of TUH and its services, he is also the patient representative on the Quality, Safety & Risk Management Board Committee (QSRM) for the Hospital.  Colette Spears – Community Representative |
Colette Spears, Traveller Primary Health Care Project Co-ordinator, with Tallaght Travellers Community Development Project. The Project works with over 200 families across Tallaght doing health promotion particularly on cardiovascular disease, diabetes and on mental health services. Colette has a long history of working with Travellers to address the social determinants of health such as access to quality health care services and for culturally appropriate accommodation.  Samantha Griffin – Community Representative |
Samantha is the Coordinator of the Tallaght Health Project, role for over four years, she has a degree in Addiction & Community Development and a strong background in mental health, addiction, and community engagement. She previously worked as a Roma Housing & Health Worker in Tallaght for two years and served as a manager with Sophia Housing, supporting individuals and families experiencing homelessness.
Having grown up in Tallaght, Samantha is deeply passionate about promoting positive health & wellbeing in her community. She leads a range of inclusive health programmes tailored to local needs, coordinates the We Can Quit programme for the area, and hosts the annual Tallaght Health Fair. Through both professional expertise and lived experience, she is committed to empowering marginalised groups and fostering a healthier, more connected community.  | Áine Lynch - Director of Nursing & Integrated, Tallaght University Hospital |
Áine moved from the Adelaide Hospital to TUH on the day it opened on June 21 st 1998. She has spent almost two decades working in several positions at Tallaght including Clinical Nurse Manager II in Trauma Orthopaedics, Clinical Facilitator in Orthopaedic Nursing, Nurse Practice Development Advisor and Nurse Practice Development Co-ordinator in the Adult Services. In her earlier career, she also spent five years working abroad in both the UK and Saudi Arabia. She moved from Tallaght University Hospital to the HSE in 2016 for just over a year where she initially worked as Nursing and Midwifery Planning and Development Officer and later held the role of Interim Director at the Nursing and Midwifery Planning and Development Unit (Dublin, South Kildare & Wicklow) for a period of nine months. This provided her with a unique opportunity to support nurses in all disciplines: midwifery, mental health, intellectual disability, public health and older persons care. Áine was very happy to return to TUH in April 2017 as she believes it maintains a strong focus on ‘people caring for people’. Along with the nursing service, she is also executive lead for the Patient Advocacy, Pastoral Care and Arts & Health Departments and the Patient and Community Advisory Council.  | Carol Mullins - Patient Advocacy Co-ordinator & Patient Experience Lead, Tallaght University Hospital |
Carol Mullins is the Patient Advocacy Co-ordinator & Patient Experience Lead for Tallaght University Hospital. In this role she represents the patients of the Hospital who want to provide feedback on their patient experience positive and negative. She deals with the medical staff in resolving any questions or queries patients have about their experience during their patient care. This Hospital service vice was established in 2002 by Carol and she remains the driving force behind the development of the service. The objectives of Patient Advocacy is to represent the patient voice, advise senior management on learnings and continuous improvement projects that can be established based on the evidence of feedback received, positive and negative. This all ultimately leads to the delivery of safer patient care which is the mission of the Hospital. Carol has over 20 years’ experience working in healthcare. She has extensive experience in the delivery of front line services having worked as Administrative Manager in the Emergency Department before undertaking her current role. She has participated in the Patient Community Advisory Council since its establishment in 2012.  | Joanne Coffey - Communications Manager, Tallaght University Hospital |
In her role as Communications Manager for the Hospital, Joanne acts as the communications link within the Hospital and also to our surrounding communities, keeping everyone informed of news and events that take place involving Tallaght University Hospital. A former volunteer tutor with the National Adult Literacy Agency, she has a great enthusiasm for keeping things simple and ensuring any information presented by the Hospital is done in an accessible way. As a member of the PCAC since 2014 she has involved the group in many different initiatives, such as the new hospital website, Know My Medicines and the Tallaght University Hospital Patient App. She makes every effort to ensure that the interests of the patient is at the forefront of everything that is developed by the Hospital. She is also the key link between the Hospital and community in developing a growing popular series of Public Health Education talks. These events bring various members of speciality medical teams out into the community to educate on various health topics and answer questions from members of the public.  | Ciaran Young - Community Representative |
Ciaran Young is a lecturer in the Department of Mechanical engineering in the Institute of Technology Tallaght. He is a former patient of the Adelaide Hospital and Tallaght University Hospital. He has been a member of PCAC since 2012 and is currently its’ vice chair, he is also the patient representative on the Sepsis Committee for the Hospital.
|
Annual Financial Statement 2024
Annual Financial Statement 2023
Annual Financial Statement 2022
Annual Financial Statement 2021
Annual Financial Statement 2020
Annual Financial Statement 2019
Annual Financial Statement 2018
|
Annual Report 2023
In 2023 the Hospital reported a 12% reduction in waiting lists. The report also revealed that 84% of patients were waiting three months or less for surgery. This is a significant achievement considering the increased activity levels and demands on hospital services during 2023.
One of the best indicators of the growth in the Hospital's workload can be seen by looking at the number of patients who attended the Emergency Department (ED) at TUH during 2023. For the first time last year over 55,000 attended the ED. On average it took 32 minutes for patients to be triaged on arrival and most were seen by a doctor within four hours and 29 minutes.
Annual Report 2022
This report highlights a significant reduction in its waiting times for daycase procedures. The Hospital’s annual report for 2022, reveals there was an 82% reduction in the number of patients waiting longer than 12 months for a daycase procedure. Overall this particular waiting list fell from 262 in January 2022 to 48 in December 2022. This was primarily as a result of the Hospital opening its new Reeves Day Surgery Centre.
Annual Report 2021
The comprehensive report outlines what was achieved by the staff, management and board of the Hospital in a year which saw the continuation of a pandemic and a crippling cyber-attack on the national healthcare system. The Hospital was fortunate that it had previously invested in the digital infrastructure protected the organisation from the conti cyber-attack, initially access to national systems were halted but the internal network continued to function. This enabled hospital staff to work with minimum disruption to patient care. Annual Report 2020
The 2020 Annual Report outlines what was achieved by the staff, management and board of the Hospital in a year of significant and unprecedented pressure on the Hospital. Despite the challenges the Hospital maintained and delivered on the Hospital’s strategy with tremendous progress made on implementation across six priority strategy areas. With a clear focus on future development the Hospital has announced plans to recruit an additional 300 staff including Nursing, Medical, Health & Social Care Professionals and Administrative staff. The plan is to recruit the additional staff over the next 12-18 months to support expansion and enhancement of services across the Hospital. Annual Report 2019
In 2019 the number of Adult ED attendances increased year on year by 3% a continuing trend for the last few years with the expectation that it will continue into the future. There were 17,886 inpatient admissions, with admissions from every county in Ireland. The number of patients over 75 years also increased by 3%. The age profile of the Hospital’s patients has transitioned from a younger population to a graduate progression to an older age profile. This demographic trend presents both challenges and opportunities for the Hospital. Year on year the inpatient and daycase waiting lists are down by 3% and 14% respectively. This reduction is a result of a combination of targeted insourcing and outsourcing initiatives. You can access the document via this link. Annual Report 2018
There were over 420,000 patient episodes of care delivered at Tallaght University Hospital (TUH) last year, according to the Hospital annual report for 2018 published today. The number of Adult Emergency Department attendances increased by 2% over the previously rear bringing the total to over 51,000. Admissions of adult patients totalled 18,694 with an increase in acuity, age and complexity of patients. There were over 32,400 attendances at the Children’s Emergency Department and over 5,574 child admissions.
Tallaght University Hospital, which celebrated its 20th anniversary in 2018, is one of the country’s largest acute teaching hospitals and a centre of excellence for a large number of specialties. A full copy of the report can be found through this link. Annual Report 2017
The 2017 annual report highlights the continued high standards of care being maintained by the Hospital despite sustained pressure to meet increasing demands with less resources.
Year on year, the Hospital has experienced an increase in emergency activity but in 2017, attendances to the adult emergency department exceeded 50,000 for the first time since opening, representing a 2% increase since 2016. In total, there were over 83,100 attendances by adults and children to the ED in 2017. The report also shows a big increase in the number of adult inpatient emergency admissions from 15,788 in 2016 to 16,349 in 2017. A full copy of the report can be found through this link. Tallaght University Hospital Annual Report 2016
Tallaght Hospital has released its 2016 Annual Report which shows that despite a significant increase in numbers attending the Emergency Department (ED). The Hospital successfully maintained its positive Patient Experience Times (PETs). While adult ED attendances rose by more than 9% (4,100+) to 49,663 in 2016 compared to 2015, half of patients were discharged within six hours and almost three quarters (72%) were discharged within nine hours. These rates were in line with 2015 figures, demonstrating that the Hospital is maintaining its high standards despite increased demand. You can access a full copy of the report through this link. Tallaght University Hospital Annual Report 2015 - People Caring for People
The 2015 Annual Report shows significant reductions in waiting times across a variety of key services, including Stroke and Endoscopy. These improvements have been welcomed by Hospital management, as evidence of the continually improving standards at the hospital while acknowledging that further improvements in access times are required. The report highlights that the average length of stay for Stroke victims fell to a two year low and Tallaght Hospital retains one of the lowest mortality rates for Stroke victims in the country. In addition, waiting times for patients requiring Endoscopies decreased by 46%, leading to increased access to urgent endoscopy where required. The report can be accessed through this link Tallaght University Hospital Annual Report 2014
TUH published its Annual Report for 2014 detailing the Hospital’s governance, performance and achievements. The Annual Report, entitled People Caring for People, reflects an emphasis on a patient centred approach to care as well as outlining the future direction of the Hospital in terms of capital investments and improved models of care. A full copy of the Report is available here
|
As a publicly funded entity TUH is accountable to the public for the provision of health services in an open and honest manner. You can read a full copy of our Board Statement on Fraud & Corruption via this link.
|
Looking towards building a sustainable, modern healing environment
Built in 1998 Tallaght University Hospital opened serving a community of approx. 62,121 people. The Hospital now services a population of over 640,000 people and is consistently operating with a deficit of beds. With census forecasting this demand will continue to increase with the number of people aged 75 or over in Tallaght increase by 322% over the next 20 years. To put this in perspective the number of people aged 75 or over in South Dublin will increase by 170% in the same time period. The Hospital has a series of planned capital developments to enhance the infrastructure and environment for patients, their families, the public and staff. This presentation outlines the Hospitals plans. Tallaght University Hospital (TUH) is a model 4, voluntary, academic teaching hospital partnered with Trinity College and situated in south west Dublin. With a staff of over 4,000 people from 63 different nationalities, it provides both acute and tertiary care to an increasing population of circa 800,000 people and is part of the newly established HSE Dublin & Midlands Region. The Hospital operates under the governance of an independent Board of Directors who give their time on a voluntary basis. TUH is also supported by the Adelaide Health Foundation, the Meath Foundation and Tallaght University Hospital Foundation. The Hospital provides access for patients to over 20 medical and surgical specialties, with comprehensive on-site Laboratory and Radiology support services. It is also a national urology centre, the second largest provider of dialysis services in the country and a regional orthopaedic trauma centre.
Tallaght University Hospital is one of two main teaching hospitals of Trinity College Dublin - specialising in the training and professional development of staff in areas such as nursing, health and social care professionals, emergency medicine and surgery, amongst many others.
Tallaght University Hospital is a Voluntary Hospital underpinned by the legal status of a Chartered Corporation established under Statutory Instrument, providing adult services and serves approximately 200 General Practitioners. Mental Health services operate on-site under HSE governance structures, with close operational alignment to the adult services provided by Tallaght Hospital. The Trinity Health Ireland (THI) collaborative agreement underpins Tallaght University Hospital’s valued relationships with Trinity College Dublin (TCD), St. James's Hospital, and the Coombe Women and Infants University Hospital. Uniquely, Tallaght University Hospital operates within two Hospital Group Structures — the Dublin Midlands Hospital Group (DMHG) and the Children’s Hospital Group (CHG) — and within Dublin South Central Primary Care Community Health Organisation (CHO) Area Seven. Tallaght University Hospital has long-standing strategic and operational alliances with Naas General Hospital and Peamount Healthcare,
among other healthcare providers within the region.
The Tallaght University Hospital Campus is 31 acres in size, with significant future development capacity, annual gross expenditure is in excess of €0.25bn. The Hospital opened on June 21st 1998 through the amalgamation of three independent voluntary hospitals: the Adelaide, the Meath and the National Children’s Hospital (NCH). Founded in 1839, the Adelaide Hospital was famous for its nursing school; the Meath Hospital, the oldest voluntary hospital and the oldest university teaching hospital in the country, was founded in 1753; and the NCH, the first dedicated children’s hospital in Ireland and Britain, was founded in 1821. The Adelaide, the Meath and the NCH have a long and proud history of providing specialist services to patients in Dublin. Many of the Hospital’s core strengths today originated from national and regional specialist services developed in these base hospitals, including; Urology, Orthopaedics, Nephrology and General Paediatric services.
|
The vision, mission and values of our hospital are: 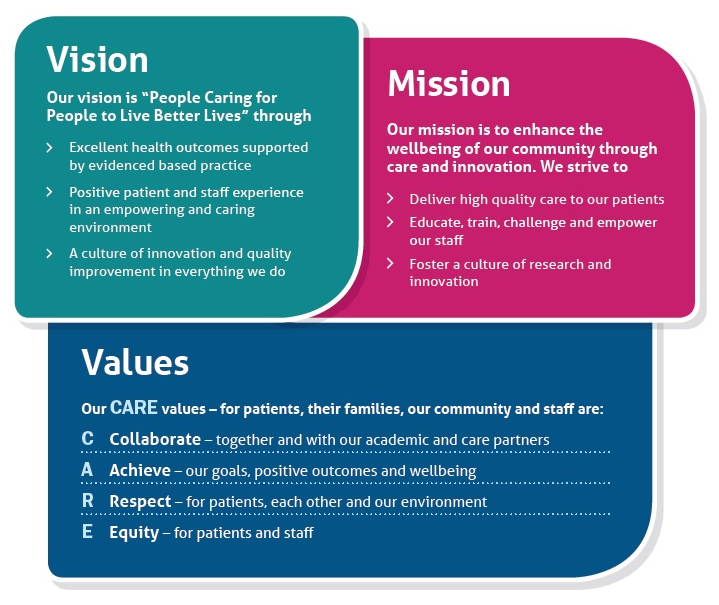
|